A lack of nitric oxide gas in the walls of blood vessels leads to a malfunction of the endothelium. This coronary artery disease reduces the size of your arteries, leading to angina or chest pain. This condition heightens the likelihood of developing cardiovascular issues, atherosclerosis, and hypertension. It requires expert diagnosis. Lifestyle changes and medications can treat it.
People with acute or stable coronary artery disease often have a problem with their endothelial function.
Individuals who are suffering from chest pain without any damage to their major blood vessels can still have a malfunctioning.
A recent study discovered that 33% of people without coronary artery disease suffer from ED, 46% of those with chronic coronary artery problems have it, and 58% of those with acute CAD have ED.
Endothelial dysfunction can be predicted by factors such as coronary artery disease, smoking, diabetes, and other cardiovascular risk elements.
Can you undo the abnormality and restore your endothelial performance to normal?
We investigate the endothelium in greater detail and give you useful information that can be applied. Here is a detailed overview of endothelial dysfunction.
What Is Endothelial Dysfunction?
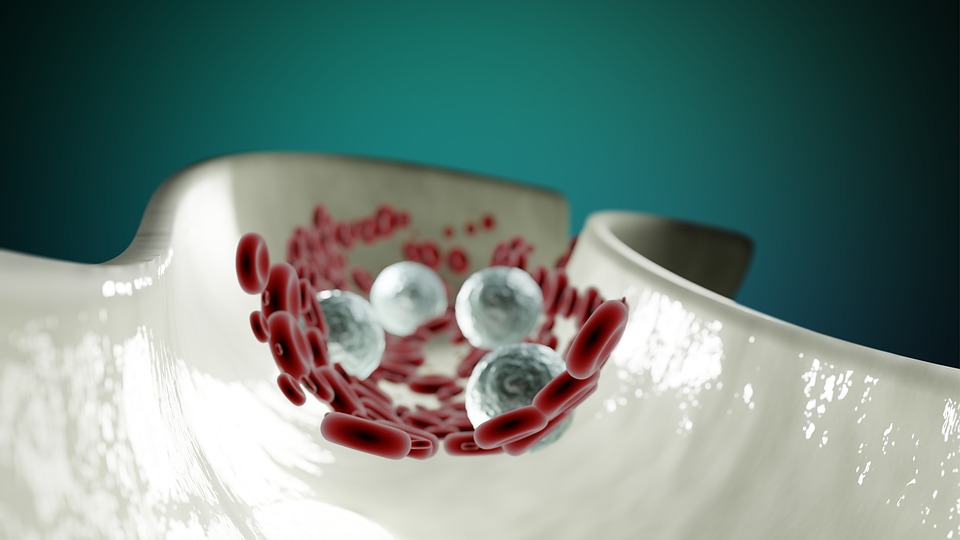
Endothelial dysfunction affects your endothelium. This thin layer of cells coats the interior of blood vessels. The cells are not functioning properly, not performing as expected. The cells cause your blood vessels to become smaller rather than remain wide open.
This condition is the result of vasospasm, which is a form of coronary artery disorder. This implies that the coronary arteries become constricted even though there is no actual obstruction. The impairment of the endothelium increases the probability of developing coronary artery disease from atherosclerosis.
What Does the Endothelium Do?
The endothelium, which is made up of a single layer of endothelial cells, covers the inside of all blood vessels, such as arteries, veins, and capillaries. This makes it one of the largest organ systems in the body.
The endothelial cells in arteries are responsible for the release of substances that regulate the contraction and relaxation of blood vessels. The amount of tension in the blood vessels controls the amount of pressure in the blood and determines how much effort the heart needs to put in to circulate the blood.
Your endothelium also:
- Controls fluids and electrolytes in your blood.
- Helps your body clot blood when needed.
- Keeps toxins out of tissues.
- Regulates tissue inflammation.
How Common Is Endothelial Dysfunction?
It was believed by health experts for a long time that the endothelium was simply a wall in the blood vessels. Once they acknowledged it as a part of the body’s internal structure, they were able to determine that endothelial malfunction was its own particular disorder.
These discoveries occurred in the late 1990s. This implies that acknowledging the situation is still relatively recent. Experts aren’t yet sure how many people develop it.
What Causes Endothelial Dysfunction?
When the amount of nitric oxide (NO) within the walls of your blood vessels is insufficient, it causes a condition called endothelial dysfunction. Your endothelium produces nitric oxide, which causes the widening of your blood vessels and allows blood to flow more easily.
A drop in nitric oxide can lead to:
- Narrowed blood vessels, which can contribute to high blood pressure.
- Inflammation in your artery walls, which can lead to atherosclerosis.
- Increased platelet production, which causes blood clots.
- Porous blood vessel walls, which expose tissues to damaging lipoproteins and other toxic substances.
What Are the Symptoms of Endothelial Dysfunction?
Chest discomfort, also known as angina, is the primary indicator of a problem with the lining of the coronary arteries. The chest pain you are experiencing is caused by your arteries becoming blocked instead of staying open. The chest pain is often worse during physical activity.
Some individuals experience angina even when they are not active, which can be a sign of a heart attack. Signs of the condition include persistent chest discomfort, extreme weariness and difficulty breathing. This is a medical emergency that requires immediate treatment.
What Are the Risk Factors for Endothelial Dysfunction?
Certain factors may increase your risk of endothelial dysfunction. Your risk is higher if you have:
- Diabetes.
- High blood pressure (hypertension).
- High blood sugar (hyperglycemia).
- High cholesterol.
- Metabolic syndrome.
- Smoking.
- Obesity.
- Certain autoimmune diseases.
What Conditions Are Linked to Endothelial Dysfunction?
Endothelial dysfunction increases the risk of cardiovascular diseases and other conditions like:
- Atherosclerosis and coronary artery disease.
- Blood clots and strokes.
- Enlarged heart (hypertrophic cardiomyopathy).
- Heart attacks and heart failure.
- High blood pressure (hypertension).
- Kidney failure.
- Peripheral artery disease (PAD).
- Pulmonary hypertension (PH).
- Small vessel disease (coronary microvascular disease).
What Are the Complications of Endothelial Dysfunction?
Endothelial dysfunction can lead to acute coronary syndrome. The amalgamation of three distinct kinds of coronary artery illness augments the likelihood of a plaque breaking apart inside a vessel that carries blood. A broken plaque can prevent the flow of blood to the heart muscle, leading to a heart attack.
How Is Endothelial Dysfunction Diagnosed?
Medical professionals employ imaging tests to observe the circulation of blood through the arteries directly. These examinations enable your healthcare provider to detect indications of endothelial dysfunction. These tests include:
- Electrocardiogram (EKG).
- Angiogram, including coronary computed tomography angiogram (CCTA).
Doctors may employ certain forms of stress imaging to determine if there is a lack of blood flowing through the blood vessels that can lead to a decrease in the performance of the heart. These imaging tests include:
- Echocardiogram (echo).
- MRI.
- Positron emission tomography (PET) scan.
How Is Endothelial Dysfunction Treated?
If you have coronary or peripheral artery disease due to endothelial dysfunction, your healthcare provider may also recommend medications, such as:
- Aspirin or medications to prevent blood clots.
- Blood pressure medicines like calcium channel blockers.
- Cholesterol-lowering drugs like statins.
- Nitrates to open up blood vessels.
If you suffer from endothelial dysfunction, you can reduce your symptoms by making alterations to your diet and daily habits. These include:
- Eating a heart-healthy diet and getting regular exercise.
- Limiting alcohol consumption.
- Losing weight (if needed) and maintaining a healthy weight.
- Finding healthy ways to manage stress.
- Getting help to quit smoking and avoiding secondhand smoke.
- Managing conditions like high blood pressure, diabetes and high cholesterol.
What Is the Outlook for People with Endothelial Dysfunction?
It is possible to manage endothelial dysfunction effectively by making modifications to one’s lifestyle and taking the necessary medications. Despite treatments, some people with nonobstructive coronary artery disease still experience chest pain.
Chronic chest pain can interfere with daily activities. It may lead to anxiety and depression. Psychotherapy, medication and stress management techniques can help.
Can You Reverse Endothelial Dysfunction?
Recent studies indicate that it might be possible to reverse problems with the inner lining of the blood vessels with certain intervention methods.
It is possible that either natural remedies or prescribed medications may be advantageous for the arteries and blood. Further research is needed to determine the sustainability and lasting impact of these findings.
Certain medications may be able to enhance the functionality of the blood vessels’ lining after a period of six months. Experts need to explore further whether the changes to the arteries, endothelium, and blood circulation can give an advantage to the coronary artery. And provide a clinical benefit.
Many studies have been conducted to examine the enhancement of the endothelium’s functionality during the initial stages of atherosclerosis. Mainly in young adults and children.
If the dysfunction is identified in its initial stages, there is a higher chance of it being able to be reversed. At an early stage, if people with illnesses implemented plans to maintain their endothelial cells in good condition, they could improve their overall health.
How to Reverse Endothelial Dysfunction
Articles that are related to each other discuss the connection between the endothelium and heart disease. However, not many pay attention to how to fix endothelial dysfunction.
People who have knowledge of how the vascular endothelium affects nitric oxide are better able to come up with a solution for the dysfunction.
Natural Methods
Experts have discussed the incorporation of food components. This includes both supplements and substances naturally found in the body that assist in regulating the lining of the blood vessels.
Studies have indicated that certain natural products and food may be beneficial for improving vascular and endothelial health.
Issues with the endothelium can cause serious heart disease. This can also cause an imbalance in oxidants and free radicals, which can have a drastic effect on the endothelial cells.
It is essential for individuals who are prone to heart disease or blood flow issues to monitor the condition of the coronary artery.
1. Food and Diet
Studies on animals suggest that foods high in polyphenols and products made from food can help to trigger activities in the cells that line blood vessels. And promote a better nitric oxide formation.
These options include red berries, blackberries, and grape-derived products. Alternative choices are hot chocolate, dark tea, green tea, and omega 3 fatty acids.
The consumption of these products displayed a betterment in endothelial dysfunction, especially among people with heart disease.
This review, even though it is experimental and restricted, suggests that natural products may have the capacity to reverse the situation. Predominantly for those at risk of coronary heart disease.
Patients who are at risk of heart disease and require maintaining their endothelial function should be encouraged to consume nutritious food.
Consuming ginger, oily fish, nuts, walnuts, berries, and garlic can boost blood circulation.
2. Physical Activity
Exercising is required to bring back the correct circulation of blood. Working out can help control the issues and lessen some of the extra weight.
3. Quit Smoking
Those with endothelial issues are urged to quit smoking. Smoking produces a buildup of plaque in the arteries, making it difficult for the heart muscle to perform correctly.
4. Manage Stress
Stress is another thing to manage. Tension can have a major effect on the circulation of blood and the cardiac muscle. If neglected for an extended period, one’s blood could become thicker, increasing the possibility of developing heart problems.
If you’re unsure of where to begin, seek advice from an expert. They can advise you to start exercise counseling. Include nutritious meals in your diet, learn ways to manage your stress levels, and take medication if it is needed.
5. Vitamins
The BioMed Research International Journal suggested that tetrahydrobiopterin, antioxidants, and vitamins could be beneficial in stimulating endothelial progenitor cells. Additional reports seem to support these claims.
The American Heart Association’s Journal reported that vitamins C and E are necessary for maintaining the genetic endothelial function of the enzyme eNOS and the NADPH oxidase activities.
Vitamin C and E, which are both antioxidants, have been found to enhance endothelial function in both animals and humans. Vitamin C, either by itself or combined with Vitamin E, has been demonstrated to increase the production of nitric oxide and reduce blood pressure in animals with hypertension.
In conclusion, certain levels of vitamin C can improve the problems with blood vessels that are associated with hypertension and congestive heart failure.
Research results regarding vitamin E’s effects on the endothelium are inconclusive. Evidence suggests that oxidative stress plays a role in the way genetic vascular dysfunction develops.
Experts suggest that taking a higher dosage of vitamin E than vitamin C may improve the patient’s vascular function and relaxation, as well as provide better endothelial function.
An increase in nitric oxide production was associated with these results. Vitamin C is seen as a significant water-soluble antioxidant with the ability to reduce oxidative stress. Utilizing it for the inner lining of blood vessels can also be advantageous.
Medical Treatments
Medication
Studies suggest that statins and other cholesterol-lowering medications may be beneficial for medical treatments. In addition to calcium channel blockers, angiotensin receptor antagonists, L-arginine, erythropoietin, and thiazolidinediones are also used.
These results were seen in clinical trials. ACE inhibitors that are taken regularly may help improve the way blood vessels function in people with a risk of cardiovascular problems.
Blood flow can be increased, which in turn can lead to widening of the blood vessels due to endothelial cell activation. It increases the forces on the endothelium that cause it to tear.
mRNA Expression
A study conducted in 2016 demonstrated that a thorough understanding of how mRNA expression works could provide novel treatments and indicators to help regulate endothelial function. The main issue linked to elevated blood pressure and heart disease problems.
Aortic Rings
An additional study conducted a more thorough analysis of impaired endothelial functioning in rings taken from the aorta. It was discovered by scientists that protein kinase C plays a significant part in the disorder brought on by high blood pressure. Administration of sodium nitroprusside helps enhance the performance of the endothelium in rings that are not working correctly.
When Should I Call the Doctor?
Call your healthcare provider if you experience:
- Chest pain.
- Shortness of breath.
- Signs of a heart attack.
- Unexplained fatigue.
What Should I Ask My Provider?
You may want to ask your healthcare provider:
- What caused the endothelial dysfunction?
- Do I need medications?
- What lifestyle and dietary changes should I make?
- Am I at risk for heart disease? How can I lower this risk?
- Should I look out for signs of complications?
Conclusion
Endothelial dysfunction is a type of coronary artery disease. When there is not enough nitric oxide gas in the walls of your veins and arteries, the arteries will become constricted. This narrowing slows blood flow to your heart. The condition can lead to chest pains known as angina and raises the likelihood of developing heart issues. Medical professionals with a lot of experience can recognize signs and carry out imaging tests to determine a diagnosis. You can alter your habits and eating habits, as well as take medications, to address endothelial dysfunction. You can reduce your chances of having serious cardiovascular issues by following these steps.
Using natural methods is the best way to ensure that the heart is in optimal condition. This provides patients with an effective way to prevent heart problems.
Medication takes a more thorough initiative. Only a medical professional can give this medication.
Other than that, vitamins seem to help. Like vitamin C and vitamin E. Many studies have shown that it can be beneficial for endothelial dysfunction, so it may be worth experimenting with.
People should not attempt to make drastic changes to their lifestyle by themselves. They should consult with an expert beforehand. By obtaining professional assistance, you can travel quite far and stay away from the potential of any additional medical problems.